Videos
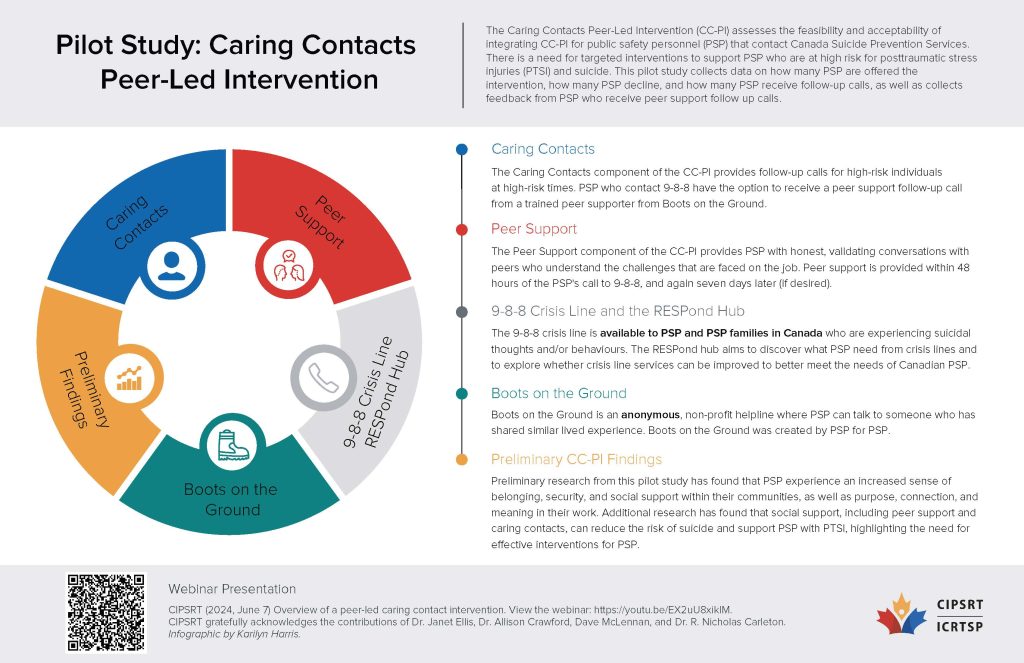
Public safety personnel and their families are disproportionately affected by suicidality and adverse mental health outcomes. There has been a strong preference for peer-led supports and informal services due to barriers to help-seeking including a culture of stoicism and mental health stigma. This webinar highlights the importance of suicide prevention and introduces a novel peer-led caring contacts intervention for public safety personnel in crisis who call a crisis line. Learn the rationale, status, and current perspectives on this ongoing study including the current efforts put forth by 988 and Boots on the Ground, and the discussion the intervention’s pillars of instilling hope, connection, and validation, with the goal of mitigating suicidality and increasing help-seeking among public safety personnel.
June 7, 2024.
What we learned
There is an urgent need for targeted interventions to help support PSP who are at high risk for posttraumatic stress injuries (PTSI) and suicide. Research has found that social support, including peer support and caring contacts, can reduce the risk of suicide and support PSP with PTSI.
Caring contacts include:
- Follow-up communications with high-risk groups at high-risk times;
- Offering encouragement;
- Fostering human connections;
- Instilling hope; and,
- Providing resources.
The current study will look at the feasibility and acceptability of integrating caring contacts and peer intervention (CC-PI) for PSP that contact Canada Suicide Prevention Services (CSPS).
Peers trained using a modified version of standard crisis training will be available to take calls from PSP in crisis. Consenting PSP will receive CC-PT within 48 hours and again within seven days following their initial call. During their interactions, the peer supporter will take detailed notes to record key themes discussed. PSP completing CC-PI will be asked to complete a post-intervention survey.
Part of the pilot program will also be to assess the peer supporters. Peer supporters will attend monthly working group meetings with the research team and be offered regular check-ins and monthly community practice support. Interviews with these peers will be completed after six months to explore CC-PI experiences and recommendations for improvement.
Should the project succeed, the researchers believe they will have a scalable and cost-effective program to prevent suicide and support PTSI in high-risk PSP. They also think it will make CSPS more meaningful and relevant for PSP.
Presented by:
Dr. Janet Ellis
Sunnybrook Hospital
Dr. Allison Crawford
University of Toronto
Dave McLennan
Boots on the Ground
Dr. R. Nicholas Carleton
University of Regina